Barbara, Don & Ray Ballard
03/24/01
My name is Barbara Ballard and my husband is Don. Our son, Ray, was born on 1/1/94. At the time he was a healthy little boy with great APGAR scores. At birth his skin was  somewhat dry and flaky, but there were no other problems. The first several months of his life were relatively uneventful. He had the usual doctor visit check ups, and received his immunizations on schedule. This included the live polio immunization. I was nursing him, and he was gaining weight, and gaining in percentile. His skin did continue to have a rash like appearance. Most of this rash was on his face. His pediatrician felt that it was most likely an allergy. We hoped that it would be something that he would outgrow.
somewhat dry and flaky, but there were no other problems. The first several months of his life were relatively uneventful. He had the usual doctor visit check ups, and received his immunizations on schedule. This included the live polio immunization. I was nursing him, and he was gaining weight, and gaining in percentile. His skin did continue to have a rash like appearance. Most of this rash was on his face. His pediatrician felt that it was most likely an allergy. We hoped that it would be something that he would outgrow.
Beginning around the age of five months, Ray began having sinus and eye infections. They were never severe and a 10 day run of antibiotics seemed to knock out the infection. 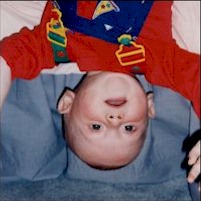 Ray was still eating and growing well. From the age of five months to ten months, he was moving to table food, and he continued to gain in percentile despite the recurrent infections. After repeated infections, I began to fear that he had an infection which was resistant to the various antibiotics which he had been given. The pediatrician began trying to culture the nasal secretions to find a resistant bug. The cultures showed little more than a common sinus infection.
Ray was still eating and growing well. From the age of five months to ten months, he was moving to table food, and he continued to gain in percentile despite the recurrent infections. After repeated infections, I began to fear that he had an infection which was resistant to the various antibiotics which he had been given. The pediatrician began trying to culture the nasal secretions to find a resistant bug. The cultures showed little more than a common sinus infection.
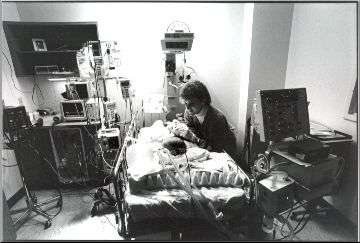
At ten and a half months old, Ray began coughing during the night. Another trip to the pediatrician showed nothing. A week later he was throwing up when trying to eat and he was pale, so we went back to the pediatrician again. This time Ray’s lips were tinged in blue, and his heart rate was accelerated. We were sent for x-rays to look for a possible heart defect. The x-rays showed the real problem. His lungs were laced in white (fluid). He had interstitial pneumonia. He was admitted to the local hospital, but after two days, we were transferred to Fairfax Hospital. His lung condition was just not responding to standard antibiotic treatment. Once there, Infectious Disease became involved and HIV tests were run along with numerous blood tests. The first night there we were transferred to PICU during the night as his oxygen saturation continued to drop. The PICU tried to avoid intubating him as long as possible. He was in a tent with 100% oxygen to keep his saturation level up. Finally, they knew that intubation was inevitable and they needed to be sure what was in his lungs. It was decided that a lung biopsy was the best way to find what was causing the lung disease. The biopsy was performed the day before Thanksgiving. That same day, five days after being hospitalized, we were told the news that he had Severe Combined Immunodeficiency. He went to surgery actually feeling better than he had in a day or two. He came back intubated. He remained on a ventilator for the next 4 months.
The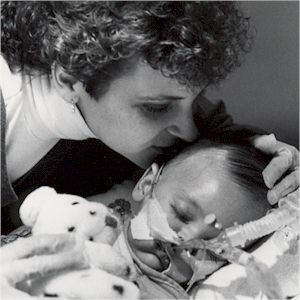 biopsy results showed that he had pneumocystis carinii pneumonia (PCP). The PICU doctors wanted to extubate him before transporting him to Duke University Medical Center in N.C., for a Bone Marrow Transplant. We spent Christmas at his bedside in the PICU. It was finally decided that he was not going to come off the ventilator without a transplant, so on December 27th he was flown to Duke and placed in their PICU.
biopsy results showed that he had pneumocystis carinii pneumonia (PCP). The PICU doctors wanted to extubate him before transporting him to Duke University Medical Center in N.C., for a Bone Marrow Transplant. We spent Christmas at his bedside in the PICU. It was finally decided that he was not going to come off the ventilator without a transplant, so on December 27th he was flown to Duke and placed in their PICU.
The next step was his BMT. That occurred on January 3rd, two days after his 1st birthday. Since Ray has no siblings, I was chosen as his donor. Several days after transplant Ray began to experience GVHD. His skin began to look like he had the measles, and then the spots began to cover his whole body. He was so red all over that he looked like a picture of the devil. His lungs were also affected by the GVHD at this time. Fluid began to collect in his lungs and his ventilatory status declined rapidly. He had to be placed on the Oscillator for the 3rd time since he had been intubated. Every day was a touch and go situation. Additionally, the hole in his lung from the biopsy still had not healed properly and he still required a chest tube. His ventilatory status wavered up and down over the next month and a half. After 13 chest tubes i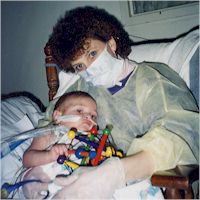 t was decided that the hole in his lung was not going to heal on its own and he would have to return to surgery to have it resewn. Since he was still on fairly high dose steroids, the plan was to wean the steroids over
t was decided that the hole in his lung was not going to heal on its own and he would have to return to surgery to have it resewn. Since he was still on fairly high dose steroids, the plan was to wean the steroids over
two weeks and then perform the surgery. Two weeks later the lung had stopped leaking and the surgery was not needed. None of the doctors were able to explain why the lung finally healed. Eventually, at the beginning of March, he was trached. Everyone was apprehensive about traching a child with SCID. The risk of infection seemed too great, but it appeared to be the only way to extubate him. He fought the vent too hard if brought to a level of consciousness where he could breath on his own.
 On March 20th, four months after he first entered PICU, Ray finally left the PICU for the step down unit. He still required breathing support but was using a bi-pap instead of a real ventilator. The consensus among the doctors was that he would require bi-pap support, at least at night, for probably a year, and that he would require oxygen support for two years. Soon thereafter we began trials to allow him time to breath on his own. By the end of April he no longer needed the bi-pap, and by the end of May he no longer needed oxygen. At the end of June his trach was removed. He had an open stoma which has never healed, probably because of his steroid use at the time, and we eventually had to have it surgically closed.
On March 20th, four months after he first entered PICU, Ray finally left the PICU for the step down unit. He still required breathing support but was using a bi-pap instead of a real ventilator. The consensus among the doctors was that he would require bi-pap support, at least at night, for probably a year, and that he would require oxygen support for two years. Soon thereafter we began trials to allow him time to breath on his own. By the end of April he no longer needed the bi-pap, and by the end of May he no longer needed oxygen. At the end of June his trach was removed. He had an open stoma which has never healed, probably because of his steroid use at the time, and we eventually had to have it surgically closed.
 During April and May, Ray also cultured out an enterovirus. Both of his two central lines had to be removed and since he was having severe diarrhea, we also had to stop the formula feeds which he had been receiving by NG tube. Prior to stopping the feeds he had begun to eat from a spoon again. Unfortunately, he only was able to eat for about one week before all of his feeding had to be stopped because the virus was attacking his GI system. He got a new central line several days later. We tried not to start him on TPN, hoping that he’d be able to tolerate the formula feeds, but that did not worked. In May he began TPN as his primary source of nutrition. It seemed that the enterovirus caused his GVHD to attack his GI track. We battled with this GVHD for many months. Ultimately, it required steroids and cyclosporine to control the GVHD. Ray is still on TPN at this time. When he began IV cyclosporine he only had a single lumen central line. An attempt was made to give him a pic line, but his veins were too fragile. He got a second central line (this was his fourth central line). One line was used for administering the cyclosporine & the other for checking the levels. One month later the newest line had to be removed due to a tract infection. Within a couple of weeks the older line clogged with lipids and had to be replaced. At that point, Ray got his fifth central line.
During April and May, Ray also cultured out an enterovirus. Both of his two central lines had to be removed and since he was having severe diarrhea, we also had to stop the formula feeds which he had been receiving by NG tube. Prior to stopping the feeds he had begun to eat from a spoon again. Unfortunately, he only was able to eat for about one week before all of his feeding had to be stopped because the virus was attacking his GI system. He got a new central line several days later. We tried not to start him on TPN, hoping that he’d be able to tolerate the formula feeds, but that did not worked. In May he began TPN as his primary source of nutrition. It seemed that the enterovirus caused his GVHD to attack his GI track. We battled with this GVHD for many months. Ultimately, it required steroids and cyclosporine to control the GVHD. Ray is still on TPN at this time. When he began IV cyclosporine he only had a single lumen central line. An attempt was made to give him a pic line, but his veins were too fragile. He got a second central line (this was his fourth central line). One line was used for administering the cyclosporine & the other for checking the levels. One month later the newest line had to be removed due to a tract infection. Within a couple of weeks the older line clogged with lipids and had to be replaced. At that point, Ray got his fifth central line.
Ray did not leave the hospital until October 4th of that year (1995). He came home on steroids, cyclosporine, TPN, Septra, and leucovorin. The next several months he was managed as if he were still in the hospital, but being at home was so much better for him physically. His strength increased and he began walking again. He finally spent his first Christmas at home. We slowly weaned him off of the cyclosporine and steroids, and once off of those we were able to stop the Septra and leucovorin. He thinned out and began growing again, but we still were not able to reduce his dependency on TPN. He had two bouts with pneumatosis in his GI tract, and also fought off another enteral virus. In March of 1996 his central line moved in the vein and was no longer in a vein large enough to support TPN. Consequently it had to be replaced and Ray got his sixth central line.
In August of ’96 while playing outside with a ball, Ray fell and cracked his left tibia. We were told that steroid use could result in reduced bone density and that this occurrence was not unlikely. By August we had also begun to realize that we were not going to make progress with his nutrition without the help of a g-tube. We returned to Duke to have the tube placed. We planned to return in eight weeks to have it exchanged for a feeding button, a more manageable type of g-tube. We ended up waiting twelve weeks because Ray had broken his left leg again. This time completely fracturing his left femur. He, amazingly, spent only two weeks in a spica cast before we were able to remove it, but we then had to keep him immobile. He spent almost all of his waking hours sitting in his stroller. After two broken legs, he became a TV, and especially, a Barney addict.
were told that steroid use could result in reduced bone density and that this occurrence was not unlikely. By August we had also begun to realize that we were not going to make progress with his nutrition without the help of a g-tube. We returned to Duke to have the tube placed. We planned to return in eight weeks to have it exchanged for a feeding button, a more manageable type of g-tube. We ended up waiting twelve weeks because Ray had broken his left leg again. This time completely fracturing his left femur. He, amazingly, spent only two weeks in a spica cast before we were able to remove it, but we then had to keep him immobile. He spent almost all of his waking hours sitting in his stroller. After two broken legs, he became a TV, and especially, a Barney addict.
 We returned to Duke just before Thanksgiving in order to have the g-tube replaced with a button. We were told that the GI doctor would endoscopy the g-tube out through his mouth and then place the button through the g-tube site. When we got to the treatment room, the doctor had changed his mind and without consulting immunology decided to use a different way to remove the tube, which was to pull it through the tract. A week later Ray was diagnosed with peritonitis. The removal of the g-tube had ripped a hole in his stomach and the new button was flushing fluids into his peritoneum. He was rushed back to Duke by ambulance for emergency surgery. The entire series of events is a long story which includes a full code event, and we came very close to losing Ray because of it all.
We returned to Duke just before Thanksgiving in order to have the g-tube replaced with a button. We were told that the GI doctor would endoscopy the g-tube out through his mouth and then place the button through the g-tube site. When we got to the treatment room, the doctor had changed his mind and without consulting immunology decided to use a different way to remove the tube, which was to pull it through the tract. A week later Ray was diagnosed with peritonitis. The removal of the g-tube had ripped a hole in his stomach and the new button was flushing fluids into his peritoneum. He was rushed back to Duke by ambulance for emergency surgery. The entire series of events is a long story which includes a full code event, and we came very close to losing Ray because of it all.
He is still partially dependant on TPN as a source of nutrition, but we have been ever so slowly increasing the amount which his GI tract can tolerate. I still hope that someday he’ll be able to be TPN free.
During the winter of 97/98 Ray began having problems with sinus infections.  A retest of his immune status showed a significant decrease in his lymphocyte studies. His immune status was tracked closely for the next six months, but in July 1998 Ray returned to Duke for a booster transplant. I was once again his donor. His T-cells now function at the low end of the “normal” range. He currently has no b-cells and continues monthly IVIG infusions.
A retest of his immune status showed a significant decrease in his lymphocyte studies. His immune status was tracked closely for the next six months, but in July 1998 Ray returned to Duke for a booster transplant. I was once again his donor. His T-cells now function at the low end of the “normal” range. He currently has no b-cells and continues monthly IVIG infusions.
Despite all of his complications, Ray is overall a happy child. He has overcome numerous setbacks which would have left an adult feeling hopeless. He’s lived much of his life in isolation, but in the Fall of 1999 he began Kindergarten on a part time basis. He’s being taught in a special ed setting which is able to handle his medical needs. So far, we’ve been very happy with his progress with the teachers and therapists. He receives therapy in OT, PT, and Speech. Due to his lack of socialization he’s quite shy around new people, but has shown good interaction with the other children in his class.
To read how his hearing loss was identified, read “Hearing Loss Identified”
Barb Ballard